Q and A with Dr. Roberts COVID-19 Census and Ventilator Use
April 24, 2020
We have been presenting the Penn CHIME prediction model each week to show the public where we stand regarding social distancing and the impact on the hospital. Why did we change this week?
As we progress further into the COVID-19 pandemic, our local experience increases in importance and the prediction models become less applicable, and potentially more confusing as we saw last week. For this week’s update, we chose to present this line graph depicting our actual number of positive and pending cases at EAMC and EAMC-Lanier since March 26.
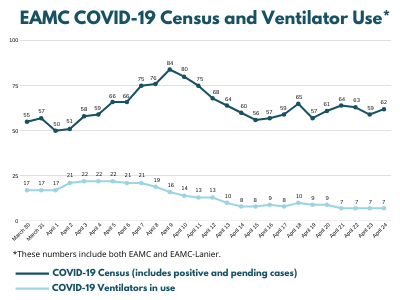
EAMC COVID-19 Census and Ventilator Use
The graph also shows the number of ventilators in use each day for COVID patients. Thinking back to our Penn CHIME model, at 75% social distancing, which I believe is close to the level of social distancing we have achieved, the predicted peak hospital census would have been around April 5-8. That chart showed we would have had a census of 100 patients with COVID-19, and around 40 of them would have required ventilators.
While we peaked close to that time frame, our hospital census was never quite that high. At this point, predictions that use a level of social distancing that is either far greater or far less than what we achieved locally are likely to be inaccurate, and we feel it is more important to focus on our actual experience here.
Why has there been such a dramatic decrease in the number of patients on ventilators?
Multiple factors have led to a decreasing proportion of our COVID-19 patients requiring respiratory support with ventilators. In the initial wave of COVID-19 patients at EAMC, many of them became very sick very quickly. They had rapidly increasing oxygen requirements which could not be met with usual supportive measures, and they had to be put on ventilators.
As this pandemic has evolved, we have become more accustomed to recognizing the early symptoms of COVID-19, and we have more of an opportunity to make adjustments which may head off severe respiratory failure. You have to remember that 6 weeks ago, no physician on our staff (or in our state, for that matter) had ever cared for a patient with COVID-19.
We are all highly motivated and we are learning every day. We have continued to make adjustments to our management strategies for COVID-19 patients based on our experiences here as well as information we receive from our colleagues around the country. This has also allowed more patients to recover from COVID-19 without requiring ventilators.
When is this all going to be over?
This is one of the most common questions I receive. When COVID-19 entered our community, the number of very sick patients requiring hospitalization increased rapidly. We admitted our first patient with COVID-19 on March 16. By April 9, we had 84 positive or pending COVID-19 patients in the hospital. From April 3-5, we had 22 patients on ventilators and our critically ill COVID-19 patients spilled into a second dedicated ICU. At the time, we did not know how much worse it was going to get, but now we believe that the week of April 5-12 was our peak for COVID-19 hospitalizations.
Unfortunately, COVID-19 does not leave a community the same way it enters. The number of COVID-19 patients at EAMC is expected to ebb and flow over the next few months. Temporary increases in patients may follow events like Easter, when people gather in larger numbers. We expect to have COVID-19 cases at EAMC for some time, and though we hope to see those numbers gradually decline, it will not be as fast as any of us wish. Social distancing has been effective in “flattening the curve” in east Alabama. It remains an important strategy in managing COVID-19 in our region.
Michael Roberts, M.D., is a hospitalist at EAMC and is the hospital’s current Chief of Staff.

Michael Roberts, M.D.